Concept Map
Name: Capella University
Instructor’s name
November, 2023
Concept Map
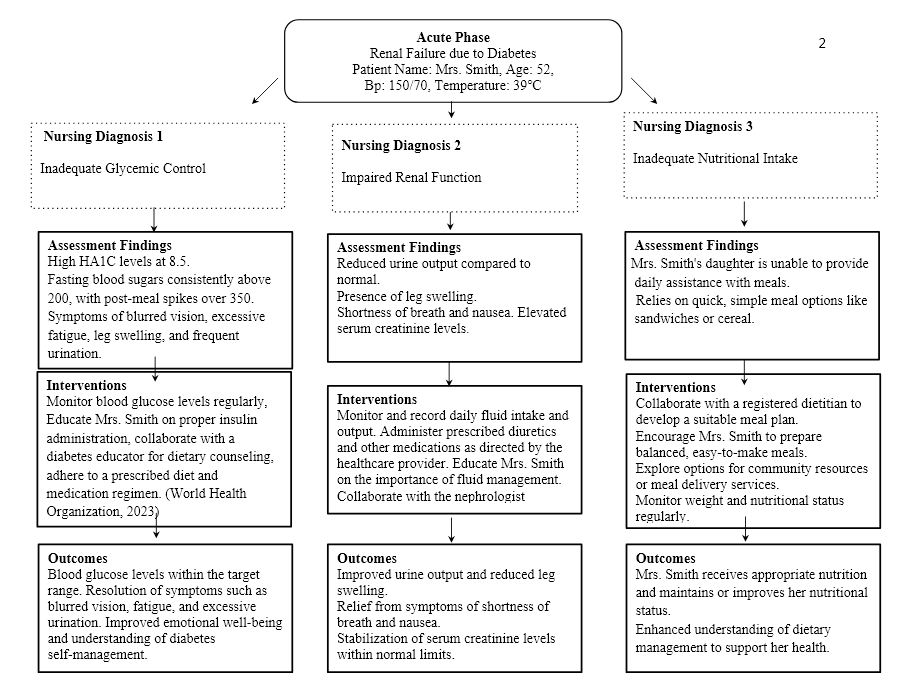
Creating an evidence-based concept map for a patient with renal failure related to diabetes in both an acute care facility and the community involves a comprehensive and patient-centered approach. In the acute care setting, the initial focus should be on stabilizing the patient and addressing acute issues. For this, nursing diagnoses such as “Acute Pain” related to renal dysfunction, “Fluid Volume Excess” related to renal impairment, and “Imbalanced Nutrition: Less Than Body Requirements” related to dietary modifications might be appropriate. Interventions may include pain management, administering diuretics, and dietary counseling. The goal in the acute phase is to stabilize the patient’s condition and ensure they are ready for transition to the community (Ganann, 2021).
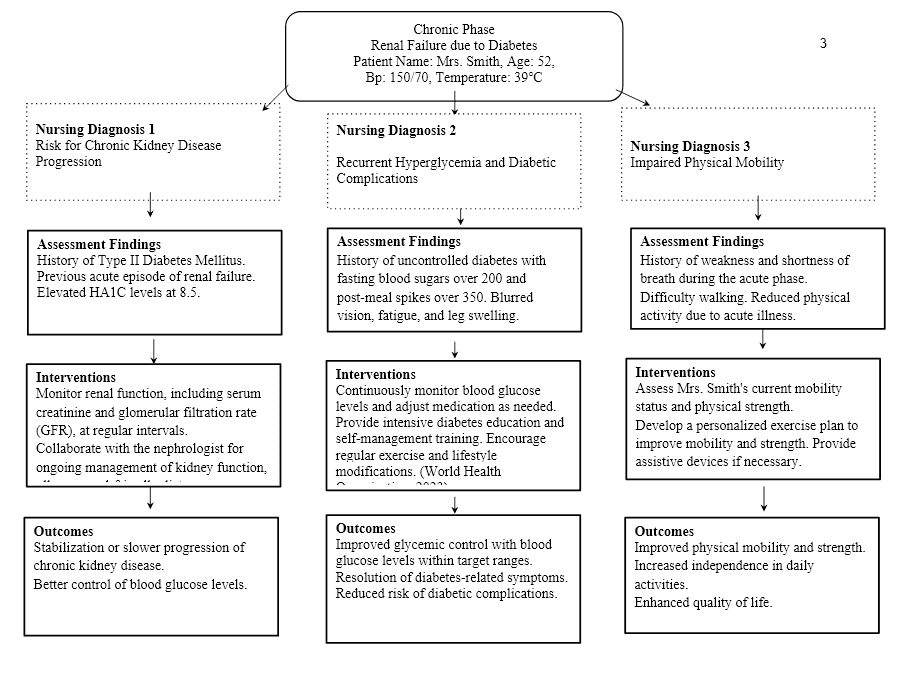
In the community, the emphasis shifts toward long-term management. Nursing diagnoses such as “Deficient Knowledge” related to diabetes self-management, “Risk for Complications” related to long-term effects of diabetes and renal failure, and “Ineffective Health Management” related to maintaining overall health while managing chronic conditions may be relevant. Interventions should focus on patient education, regular monitoring, and support for self-care (Sibounheuang et al., 2019). Achieving high-quality outcomes in this stage involves empowering the patient to take an active role in managing their health, adhering to the treatment plan, and preventing complications. This comprehensive concept map will address the patient’s needs throughout their healthcare journey, ensuring continuity of care and optimal outcomes.
Additional Evidence
The justification for the value and relevance of the evidence used as the basis for a concept map is essential to ensure that the care plan is well-informed and effective. Evidence-based practice (EBP) relies on the integration of the best available evidence, clinical expertise, and patient preferences. In the context of nursing, the evidence may come from research studies, clinical guidelines, expert opinions, and patient experiences. The incorporation of high-quality evidence into the concept map serves as a foundation for decision-making, ultimately enhancing patient care (Alatawi et al., 2020).
Impartially considering conflicting data and other perspectives is a crucial aspect of EBP. It helps healthcare professionals to critically evaluate the quality and strength of evidence, recognizing that not all evidence is of equal value. It also allows for a more holistic understanding of a patient’s situation. By acknowledging conflicting data and various perspectives, the concept map can become a more comprehensive tool for care planning. It enables nurses to make informed decisions and adjustments in a patient’s care plan, fostering adaptability and responsiveness to changing circumstances (I. Ahmed & A. Mohamed, 2019). Moreover, it promotes a patient-centered approach where the individual’s unique needs and preferences are taken into account.
Interprofessional Strategies Applied to Concept Map
Interprofessional strategies play a pivotal role in achieving the desired outcomes outlined in the concept map for a patient with renal failure related to diabetes. Collaborative efforts among healthcare professionals, such as nurses, physicians, dietitians, and pharmacists, are crucial for delivering comprehensive care and addressing the complexity of the patient’s health condition (Lee et al., 2021). By integrating knowledge and expertise from various disciplines, a more holistic and patient-centered approach can be established. This approach enhances the patient’s overall care experience and contributes to better outcomes. For example, an interprofessional team can collectively develop a tailored care plan that includes medication management, dietary guidance, physical therapy, and emotional support. Such collaborative efforts can help optimize blood glucose control, manage renal function, and prevent complications (Lee et al., 2021).
However, it’s essential to acknowledge that knowledge gaps and uncertainties may exist within the interprofessional strategies. These gaps can result from variations in professional perspectives, evolving medical research, or individual patient characteristics. In the concept map, identifying these knowledge gaps and uncertainties is crucial for effective care. For instance, when adjusting a patient’s medication regimen, the team may encounter uncertainties about the most appropriate dosages or drug interactions. In such cases, seeking consultation with specialists or conducting further research may be necessary to make informed decisions. Additionally, while interprofessional collaboration is essential, ensuring effective communication and shared decision-making among team members is vital to address any unknowns or missing information. Furthermore, interprofessional education and training are essential to fostering effective teamwork and communication among healthcare providers, as it can bridge knowledge gaps and promote a more unified approach to patient care (Pantha et al., 2021). Overall, identifying and addressing knowledge gaps and uncertainties in the concept map can lead to more precise and patient-centric care, ultimately enhancing the achievement of desired outcomes.
Conclusion
The concept map presented in this assessment serves as a comprehensive and evidence-based roadmap for the care of a patient with renal failure related to diabetes in both acute care and community settings. It highlights the importance of addressing acute and chronic phases, focusing on critical nursing diagnoses, interventions, and outcomes. Interprofessional collaboration is recognized as a key driver of desired outcomes, promoting a holistic and patient-centered approach. While acknowledging knowledge gaps and uncertainties, this concept map underscores the need for continuous learning and communication among healthcare professionals to ensure the highest quality of care throughout the patient’s healthcare journey. By embracing the principles of evidence-based practice, this concept map guides healthcare professionals in making informed, adaptable, and patient-focused decisions, ultimately leading to improved patient outcomes and quality of life.
References
Alatawi, M., Aljuhani, E., Alsufiany, F., Aleid, K., Rawah, R., Aljanabi, S., & Banakhar, M. (2020). Barriers of implementing evidence-based practice in nursing profession: A literature review. American Journal of Nursing Science, 9(1), 35–42. https://doi.org/10.11648/j.ajns.20200901.16
Ganann, R. (2021). An integrated hospital-to-home transitional care intervention for older adults with multimorbidity and depressive symptoms: A pragmatic effectiveness-implementation trial. International Journal of Integrated Care, 21(S1), 134. https://ijic.org/articles/10.5334/ijic.ICIC2063
I. Ahmed, A., & A. Mohamed, R. (2019). Undergraduate nursing students’ experience in studying evidence-based practice by application of concept map. American Journal of Nursing Research, 7(4), 437–444. https://pubs.sciepub.com/ajnr/7/4/5/index.html
Lee, J. K., McCutcheon, L. R. M., Fazel, M. T., Cooley, J. H., & Slack, M. K. (2021). Assessment of interprofessional collaborative practices and outcomes in adults with diabetes and hypertension in primary care: A systematic review and meta-analysis. JAMA Network Open, 4(2), e2036725. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2776302
Pantha, S., Jones, M., & Gray, R. (2021). Stakeholders’ perceptions of how nurse-physician communication may impact patient care: Protocol for a concept mapping study. Journal of Interprofessional Care, 1–3. https://www.tandfonline.com/doi/full/10.1080/13561820.2021.1923466
Sibounheuang, P., Olson, P. S., & Kittiboonyakun, P. (2019). Patients’ and healthcare providers’ perspectives on diabetes management: A systematic review of qualitative studies. Research in Social and Administrative Pharmacy, 16(7). https://doi.org/10.1016/j.sapharm.2019.09.001
World Health Organization. (2023, April 5). Diabetes. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/diabetes
Table of Contents
Toggle